Hot Topic Blog - Treatment & Recovery
THE JOURNEY OF AN SLP MOM~Shared by Donna Edwards, MA, CCC-SLP, BRS-S from OhioNovember 2013 |
|||
|
In this life we all have our journey…..
Having had a beloved independent aunt without sight taught me that function was the key for autonomy and optimizing skills despite personal challenges. This strong personal attachment reinforced my perception of the depth of patient input as a rich resource to guide successful return-to-life skills after a medical insult. As a speech-language pathologist (SLP) I have always felt that patient and family advocacy were a priority. I encouraged my patients and families to verbalize their needs to care providers, as well as to each other because medical diagnoses can shift family roles - often times abruptly with catastrophic events. Such thinking led to my volunteer work as the Director of Legislative Advocacy for our state association, OSLHA (Ohio Speech-Language-Hearing Association).
My clinical picture has always viewed the adult or child in my care as a family member. I saw my mother, my brother, my grandmother, my infant in the critical care bed or in the outpatient setting/chair.
Still…..
Traumatic Brain Injury (TBI) and Cerebral Vascular Accident (CVA) were not thoughts or diagnoses I had associated with my healthy, athletic, active 12-year-old son. “Get here as fast as you can, but we can’t promise he’ll still be here when you get here.” My heart stopped beating as I began to comprehend what I had just heard. “We cut off his orthodontics for imaging.” “If he survives 72 hours, he will live.” “We can’t risk a craniotomy.” I was told he must have hit his head as he fell when the spontaneous hemorrhage occurred.
As a clinician and a mother, I searched for the rationale behind my son’s two cerebral hemorrhages that covered the entire left hemisphere of his brain - leaving him in a coma, at risk for herniation at the brainstem, and in a ventilator-dependent state. My clinician’s brain told me he would probably become non-verbal, have significant cognitive decline, and not have the future we as parents tend to foresee for our children as they approach adolescence. To the surprise of the medical team, he survived his catastrophic injury. And, it was deemed that he would survive placement of a gastrostomy tube (G-Tube) and tracheostomy as he transitioned to his second intensive care unit. Nutrition was now on board, and hyperoxygenation could be reduced.
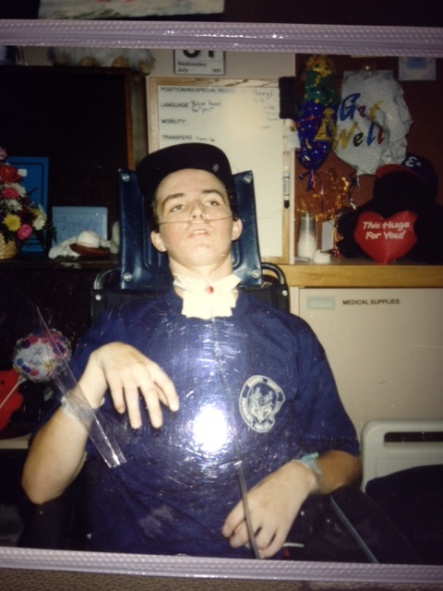
Over months of recovery, his level of alertness increased and he became more interactive with his environment. I searched earnestly for signs of improvement. Our world was crushed with his facial hypotonia, flat affect, and lack of the bright, spontaneous smile that we had come to love. Dysphagia (a swallowing disorder) was acutely obvious with his lack of tongue and lip movement and lack of saliva management. Withdrawal from the strong medications that had saved his life tore at his body and left large dark circles under his eyes and a fragile shell of his former athletic body. His treating hospital shared that they did not see complicated patients, so they recommended a nursing home for him.
After 4 weeks on a ventilator in intensive care, he could be transferred out-of-state to a Level 1 Trauma hospital that served a variety of patients on a rehabilitation unit. We were blessed yet again as the paramedics, who took him for his initial hospital stay, volunteered to transport him to the out-of-state facility free of charge. God indeed had us in the palm of his hand. Fatigued, yet full of faith, we pressed on. After arriving at the new hospital, a transfer back to an acute-care hospital setting was pondered for the first few days. However, as my son stayed awake longer, he was finally appropriate for the initiation of therapy and a low-level rehabilitation stay.
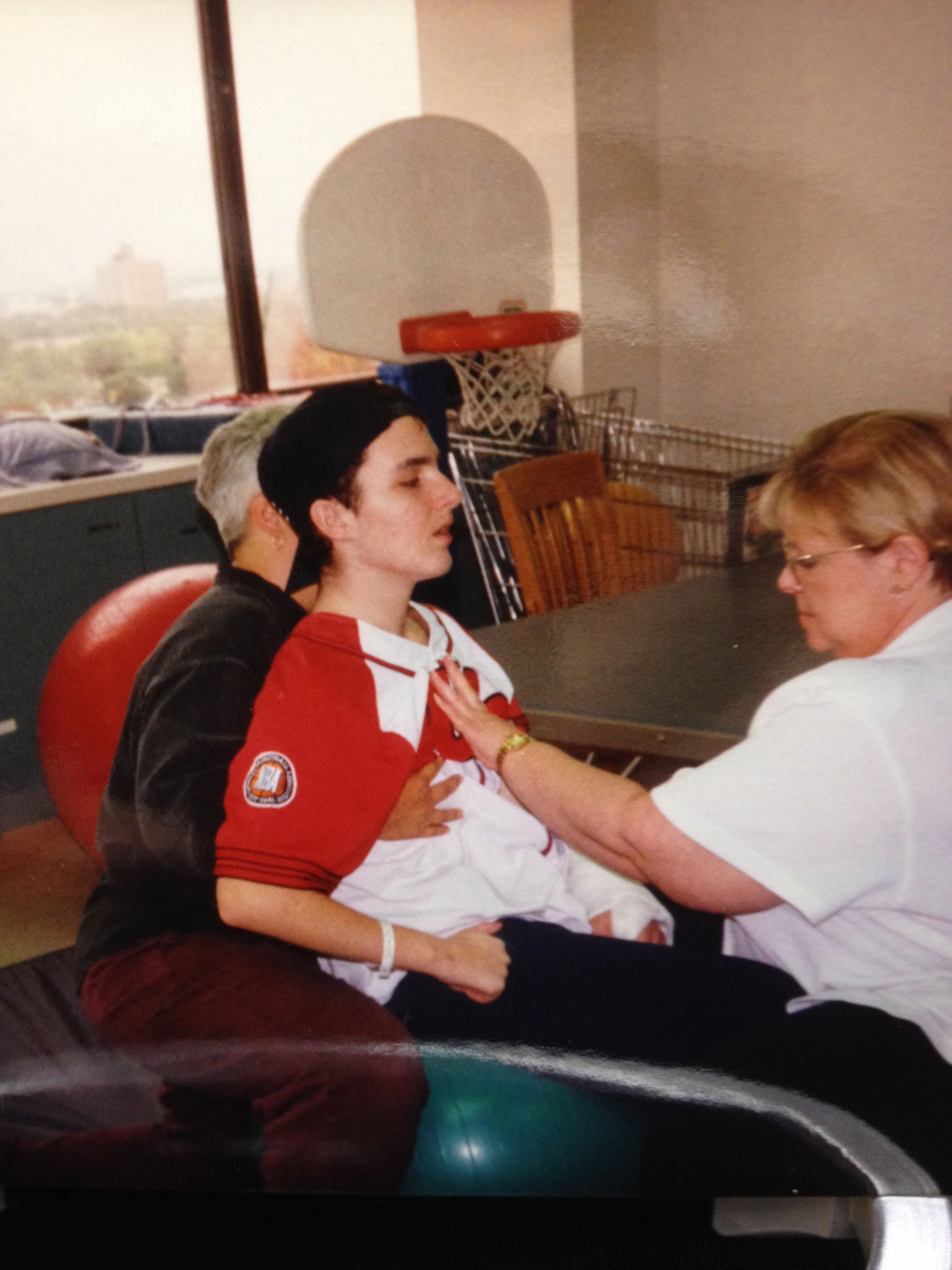
He received physical, occupational, and speech-language therapies daily. We were blessed to have clinicians trained in Neurodevelopmental Treatment (NDT) working with him individually and in co-treatments. For those of you who know the work of Leslie Faye Davis (a well-known and dedicated NDT instructor): “To get to the lips,” we indeed had to “go through the hips.” Aggressive work was done to build his core strength, so he could better control his posture and his extremities. It wasn’t long before he could hold his head up and began to participate in an increasing number of daily interactions.
His inappropriate behaviors, related to his head injury, came and went. My heart was pierced as I had to watch him struggle. His eyes finally seemed to focus, but we learned that his vision was quite impaired. The hemorrhaging on the left side of his brain and edema on the right side of his brain had affected the optic nerve. He received a formal diagnosis of homonymous hemianopsia which translated to him as “I see blurry to the left, and what do you mean there is something on my right?” I can’t tell you how many times I frustrated him by walking along and turning right without telling him first. Talk about the parting of the ways and teenage frustration.
A swallow study revealed a functional pharyngeal phase swallow and confirmed severe oral dysphagia. For those who may be unfamiliar with this terminology, he could swallow food once it reached his throat but had difficulty manipulating food in his mouth. He had learned to approximate his lips with his fingers to get bilabial speech sounds (i.e., “p,” “b,” and “m”). And yes, it’s true; he ordered one of everything off the menu from the hospital’s Wendy’s restaurant. I had to lower my head and chuckle as I respectfully declined the order.
His vocal intensity was low with his reduced trunk support, and I had concern for his cough response should he need it. Despite the severity of the hemorrhages and cerebral edema, we had much of our son back. He could communicate, tease the staff, and enjoy some easy foods. Eagle eye mom kept a close watch on his positioning and oral care. It was a happy day when I took a picture of his first empty tray as his endurance and volume of oral intake increased. The doctors agreed to remove his G-tube, an uncomfortable occurrence my son says he will never forget.
We learned to refer to the site where his G-tube had once been placed as his second belly button which, of course, he teased me about as I only have one. I share these examples in the hopes of relaying the impact that using humor can have upon facing such odds. Over time, my son went to outpatient therapies. Being the athlete who would motivate himself before the big game, he played the songs Another One Bites the Dust and We are the Champions on his way to therapy sessions. He worked hard and was excited when he took second place in the state Special Olympics swim meet despite his spastic gait and tendency to drop his left foot. Despite severe left cerebral hemorrhaging where one would expect more problems on the right side of the body, he had left hemiparesis. What??? It appears most of the damage to his young body was from the cerebral edema and not the massive bleeding that had covered the entire left hemisphere. God gave us such a miracle!
He was slowly transitioned back into the school system. First home schooling, then a half day at school, followed by half regular education classes with half special education classes for tutoring, compensatory strategies, and to learn self-advocacy. His participation with the Special Olympics one summer increased his overall endurance. Eventually, he returned to a full day in regular education classes with supports for his vision. The love of reading, he previously had as a youngster, would take years to return due to limited visual fields and eyestrain. After many IEP meetings, joint efforts for socialization, and hours of class time, he graduated from high school. President Bush awarded five letters of accommodation for educational achievement to the disabled students who graduated that year. With the tears brimming in my eyes, I could hardly see him limp his way across that stage.
Though reading was difficult, he found creative comfort in writing. I would like to share one of his poems with you. Upon first reading, it is awkward, slightly disjointed ……as his TBI journey was…..and then it coalesces into an emotionally charged ending.
LEARNING FROM YOU C. HUGHART
Looking for a way Never knowing what to say Always looking for an answer But receiving only questions Attempting to find a path But yet only feeling your wrath I want to learn that is not a lie I need your help so I can fly I want to learn from you But you leave me without a clue As I look back into the past It comes to no surprise that you were last I remember how you always made me work And the way you always smirked I look back and finally saw You helped me grow mentally without a flaw I wanted to learn from you But you have helped so much… ……………………………………and I didn’t have a clue.
Tomorrow is his 30th birthday. He still snaps his left knee and has dysarthric (i.e., distorted sounding) speech when tired. Nevertheless, his undaunting spirit has seen him through a college education, job search, marriage, divorce, and the birth of his son. It has been a long road and a difficult journey, but one paved with love, faith, and endurance. With God’s grace we have survived thus far and learned to appreciate each day, each love, each season.
I hope the sharing of our story touches and encourages you. I also hope that:
For C. |
|||