Question & Answer - Oral Sensory-Motor, Myofunctional, Vocal Tract, & Airway Information
So what is the difference between functional and dysfunctional breathing?September 2019 |
|||
|
Answer from Dr. Rosalba Courtney, DO, PhD, Osteopath and International Presenter from Australia This was a key driving question in my PhD research called Dysfunctional breathing: Its parameters, measurement and clinical relevance. The real practical aim of my research was to create a standardized protocol for assessment and treatment of dysfunctional breathing. I knew from my training and clinical experience as an osteopath it’s not possible to assess or treat any condition well until you understand its characteristics and parameters well enough to define it. So firstly, let’s consider the question “What is functional breathing?” The conclusion I came to is “functional breathing is breathing that most efficiently performs its various functions taking into account the circumstances and condition of the patient.” Next question: “What are the functions of breathing?” This is an interesting question that gets more interesting the more one thinks about it because breathing has both primary and secondary functions. The primary functions of breathing are the ones essential for keeping us alive. The secondary functions of breathing are more about how breathing interacts with other body systems in ways that help to maintain homeostasis and health. The primary functions of breathing are: -Biochemical and -Biomechanical The biochemical function of breathing has to do with the regulation of oxygen, carbon dioxide, and the pH of the body. The biomechanical function of breathing relates to the action of the respiratory pump, the efficiency which is dependent on the actions of the respiratory muscles, the function of the rib cage, as well as the habits and patterns of breathing. The secondary functions of breathing refer to the involvement of breathing in things such as: -Self-regulation (i.e., calming and dealing with stress or improving mental focus, mindfulness, and attention) -Static and dynamic posture, spinal “core” stability, and motor control -Modulation and support of speech, vocalization, and upper airway function during daytime and night time breathing -Creation of rhythms or oscillations allowing systems to communicate and function together -Regulation of fluid dynamics (e.g., in cerebrospinal fluid, lymphatic circulation, venous return to the heart, and blood pressure regulation)
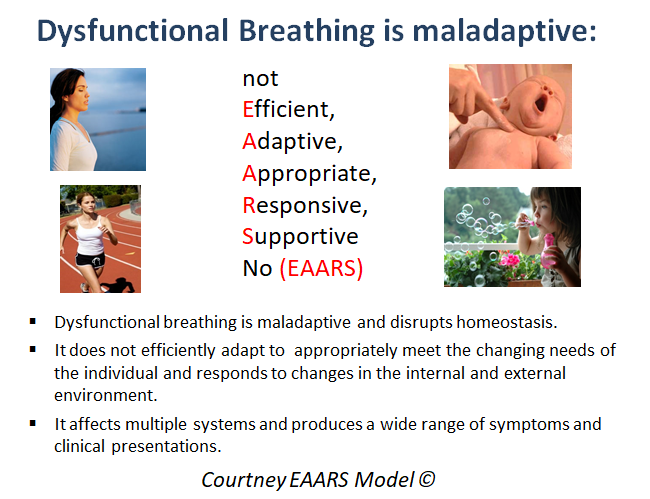
The efficiency of these secondary functions of breathing is reduced when the primary functions of breathing are not well maintained. For example, people with hyperventilation (i.e., a condition resulting in low levels of CO2 and pH disruption) or neuromuscular breathing pattern disorders often find the sensations of breathing uncomfortable and unpleasant. For these people, practicing mindful attention to the breath or attempting to control the breath in ways supposed to be calming may make them feel more agitated and even distressed. Functional breathing has EAARS - The EAARS acronym is one way to think about whether a person’s breathing is functional. EAARS stands for - Efficient, Adaptive, Appropriate, Responsive, and Supportive of health. The EAARS model acknowledges the dynamic, ever changing nature of healthy breathing, as well as the fact the way a person breaths may represent his or her best attempt to compensate for pathology, structural deficit, or even psychological state. Using the EAARS model to evaluate breathing functionality, we are concerned with how effectively the breath changes and responds to meet the body’s changing needs rather than just looking at static measures and textbook norms. The EAARS model for evaluating functional and dysfunctional breathing takes us away from rigid ideas about optimal breathing and opens up possibilities for innovative ways of approaching breathing retraining respectful of the body’s own healing and compensatory mechanisms. Here is a letter by letter detailed description of the EAARS acronym. Efficient breathing - Certain modes, rates, rhythms, or patterns of breathing are more efficient than others. However, to accurately interpret the functionality of breathing, we need to look at the whole picture. For example, generally speaking, nasal breathing is more efficient than oral breathing at delivering oxygen. Yet, there are situations where the upper airways are obstructed to the point when nasal breathing reduces oxygen and overloads the heart, so mouth breathing is more efficient at maintaining oxygen levels and therefore more functional. Adaptive and Appropriate - When a person’s breathing is functional it adapts to changing conditions appropriately. Healthy people have breathing that changes all the time, sometimes it’s more regular, sometimes it’s less so, sometimes breathing is more thoracic, and sometimes it’s more abdominal. At the most basic level, it helps to understand functional breathing is breathing that adapts appropriately to activity and rest. At rest, we should ventilate much less than during physical activity or during arousal. When breathing does not adapt to the condition of rest we might find the person’s breathing is beyond their metabolic requirements giving low CO2 – hyperventilation. His or her breathing pattern stays in the active upper thoracic configuration and does not move to the relaxed abdominal configuration when in a position of rest. Responsive - Because functional breathing is adaptive, over-control and excessive pre-occupation with one’s breathing can make it dysfunctional. Rigid ideas about what optimal breathing looks like can make it dysfunctional (e.g., always abdominal, always gentle and soft, etc.). Supportive of Health - Breathing interacts with most body systems in a two way relationship. Healthy functional breathing promotes virtuous cycles maintaining homeostasis.
In a nutshell, dysfunctional breathing doesn’t have EAARS. It’s not efficient, adaptive, appropriate, responsive, or supportive of health. It produces symptoms and contributes to vicious cycles of pathology and dysfunction in other body systems. Another conclusion from my research is dysfunctional breathing is multi-dimensional with 3 key dimensions: (i.e., biochemical, biomechanical, and psychophysiological). People with dysfunctional breathing can have dysfunction in one or several of these dimensions. Targeted treatment that’s based on accurate evaluation of each of these dimensions is the key to effective treatment of dysfunctional breathing. The multidimensional model of dysfunctional breathing and the EAARS model of breathing functionality are the guiding principles of what I call Integrative Breathing Therapy. If you want to know more about the validated assessment and treatment tools of Integrative Breathing Therapy, please consider taking my one-day course. Details are on my website. About the Author Dr. Rosalba Courtney ND, DO, PhD is an osteopath with a broad experience in breathing therapy. She was one of the first practitioners trained in the Buteyko Method in the 1990s. She received a PhD from RMIT University for her research on the topic of Dysfunctional Breathing: Its Parameters, Measurement, and Clinical Relevance in 2011. She is internationally recognized for her work in this field, having published over 15 peer reviewed articles and book chapters on this topic. Rosalba has presented at many national and international conferences. She is actively involved in research and mentoring of osteopathic students. She is renowned for her ability to synthesize complex information from the scientific literature in order to extract its practical significance for clinicians. Rosalba conducts training programs for practitioners in Integrative Breathing Therapy internationally. She practices in Sydney, Australia. Further Reading -Boulding, R., et al., Dysfunctional breathing: a review of the literature and proposal for classification. Eur Respir Rev, 2016. 25(141): p. 287-94.
-Courtney, R., Strengths, Weaknesses and Possibilities of the Buteyko Method. Biofeedback, 2008. 36(2): p. 59-63.
-Courtney, R., Functions and dysfunctions of breathing and their relationship to breathing therapy. International Journal of Osteopathic Medicine, 2009. 12: p. 78-85.
-Courtney, R., Dysfunctional Breathing: Its Parameters, Measurement and Relevance, in School of Health Sciences. 2011, RMIT: Melbourne. p. 315.
-Courtney, R., Questionnaires and manual methods for assessing breathing dysfunction, in Recongizing and Treating Breathing Disorders, B. Chaitow, Gilbert, Editor. 2014, Elsevier: London.
-Courtney, R., Breathing training for dysfunctional breathing in asthma: taking a multidimensional approach. European Respiratory Journal Open Research, 2017. 3(4): p. 00065-2017.
-Courtney, R., A Multi-Dimensional Model of Dysfunctional Breathing and Integrative Breathing Therapy - Commentary on The functions of Breathing and Its Dysfunctions and Their Relationship to Breathing Therapy. J Yoga Phys Ther, 2016. 6(257).
-Courtney, R., Management of Respiratory Dysfunction, in Textbook of Osteopathic Medicine, C. Standon and J. Mayer, Editors. 2018, Urban and Fischer. |
|||
 So what is Dysfunctional Breathing?
So what is Dysfunctional Breathing?